Proposed use
Supplementation of C3-C10 short/medium chain fatty acids in combination with bile salt hydrolase (BSH) can be used for the therapeutic treatment of recurrent C. difficile infections or its prevention.
Problem addressed
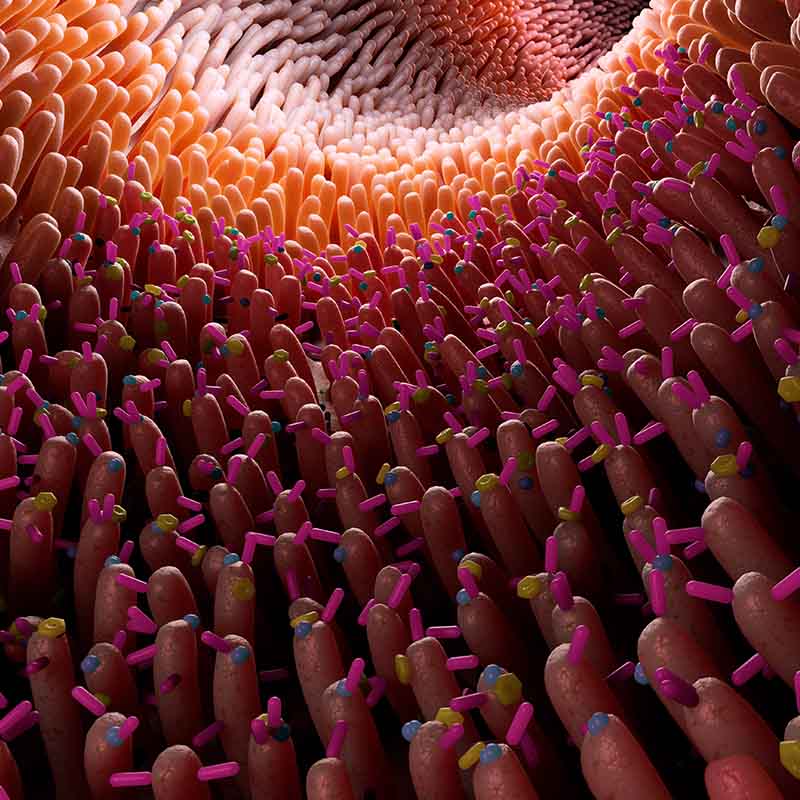
Exposure to antibiotics kills bacteria that perform important functions in the gut microbial ecosystem, resulting in a “metabolic dysbiosis” where the loss or reduction of specific microbial metabolic pathways creates an environment that promotes C. difficile germination and growth. C. difficile causes opportunistic infections in the human colon, usually after antibiotic exposure. The incidence of recurrent C. difficile infection (CDI) has disproportionately increased relative to CDI, therefore the demand for recurrent CDI therapies is rising.
The main therapeutic strategy for recurrent CDI (rCDI) is faecal microbiota transplant (FMT) which uses stool from a healthy donor to replace the microorganisms and ecosystem that are depleted in the gut of recurrent CDI patients. While FMT is highly effective at treating recurrent CDI, it is unclear whether all the microbes included in the preparations are required to resolve disease. There are concerns regarding the long-term safety, reproducibility, composition, and stability of FMT preparations. Potential risks include transmission of infections, invasive administration routes, and concerns treating high-risk individuals. As more studies describe the role of the gut microbiota in disease, it is unclear whether FMT could result in the transfer of gut microbiota which later contributes to disease. Use of BSH and the identified short to medium chain fatty acids such as valerate can treat and prevent recurrent CDI without the need of FMT.
Technology overview
Short/medium chain fatty acids such as valerate show activity against C. difficile; their combination with targeted restitution of BSH may be a novel therapy for or preventative strategy against CDI that avoids the risks of antimicrobial resistance.
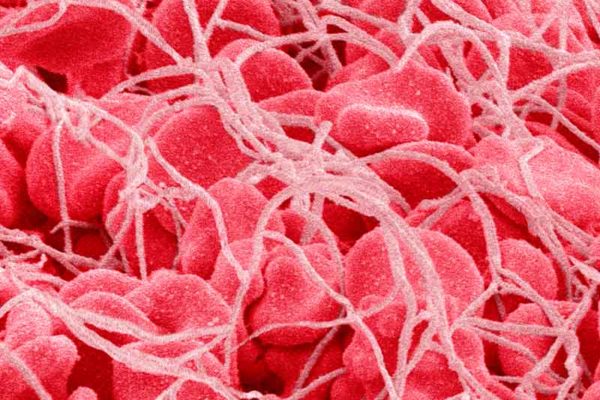
Patients successfully treated for recurrent CDI by FMT show a rapid and sustained enrichment in gut microbiota members which produce a bile metabolising enzyme, bile salt hydrolase (BSH). Relative abundance of gut BSH-producing organisms correlates negatively with stool levels of taurocholic acid (TCA), a potent trigger for C. difficile germination. TCA is hydrolysed by BSH to cholic acid; this is subsequently metabolised into deoxycholic acid, which potently inhibits the growth of C. difficile. In batch cultures, BSH-producing microorganisms completely reversed TCA-mediated germination of C. difficile. FMT functions by reversing a ‘metabolic dysbiosis’ which includes the restoration of the short chain fatty acids such as valerate, which potently inhibits the growth of C. difficile without any apparent adverse effect on gut commensal bacteria.
Further work is currently being undertaken in methods of delivery of these metabolites.
Benefits
- Negates the need to use live microorganisms, presenting a safer option
- Eliminates the need for faecal microbiota transplants and the associated difficulties
- A safe, well-defined and targeted approach of treating recurrent C. difficile infections
Intellectual property information
The invention is protected by PCT/GB2019/051052 patent application. Patent filed in EP (EP3775157A1).
Link to published paper(s)
Mullish, Benjamin H et al. “Microbial bile salt hydrolases mediate the efficacy of faecal microbiota transplant in the treatment of recurrent Clostridioides difficile infection.” Gut vol. 68,10 (2019): 1791-1800. doi:10.1136/gutjnl-2018-317842